Disclaimers
To achieve a fully holistic approach when selecting a support surface, it is essential to consider other risk factors that may not be included in the risk or skin assessment. These can include factors related to medical conditions, nutritional status, sensation, tissue perfusion, and more.
Examples:
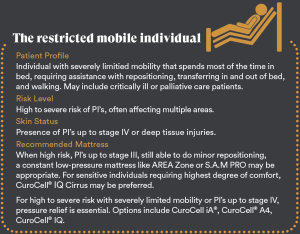
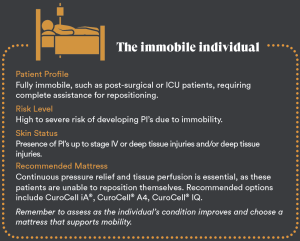
For a patient who is completely immobile and has already developed pressure ulcers/injuries, a dynamic support surface with a pulsating mode is likely the most appropriate choice for optimal prevention and treatment.
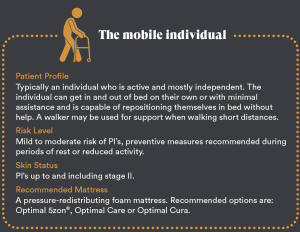
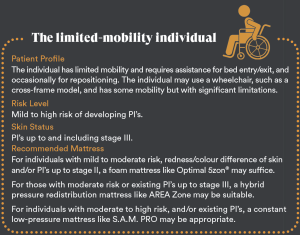
A patient assessed to be at high risk for pressure ulcers/injuries, who can walk short distances with or without assistance and reposition themselves in bed, would likely benefit most from a constant low-pressure mattress.
For a patient with intact skin or early-stage pressure ulcers/injuries, who can walk independently with or without a rollator and reposition themselves in bed, a highly specified foam mattress, such as a 5Zon, is likely suitable.
Selecting a Support Surface from a Health Economic Perspective
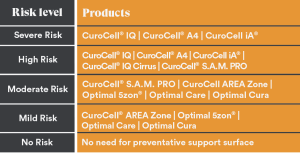
Choosing the correct support surface is important not only from a clinical perspective but also from a health economics standpoint. Using advanced and costly systems when less sophisticated, more affordable alternatives could be sufficient can lead to increased expenses for both the healthcare system and society.
Providing patients with an appropriate support surface based on their mobility and specific risk level is essential for optimizing clinical outcomes, health economics, and delivering cost-effective care.
The aSSKINg method for preventing pressure ulcers/injuries was developed by NHS Improvement in the United Kingdom. This method is part of their broader efforts to enhance patient care and prevent harm in clinical settings. The aSSKINg framework is based on a comprehensive review of existing evidence and best practices for the prevention and management of pressure ulcers/injuries. The development of the method involved synthesizing findings from multiple research studies, clinical guidelines, and expert consensus. Key components of the research and evidence base include:
Disclaimer 1: The content in “Selecting a Support Surface Based on Risk Assessment” is intended as supplementary support and does not replace the care organization’s local or national guidelines. The classification of mattress suitability is based on general product characteristics and not tailored to individual patient needs. The responsibility for prescribing the appropriate support surface lies solely with the patient’s responsible clinical professional, who must ensure that the chosen solution aligns with the patient’s unique and individual clinical needs.
Disclaimer 2: The content of this document is subject to change without notice. To ensure the correct use of each product, the product’s Instructions for Use (IFU) must always be read prior to use.
References
1. Lorraine Wright, Heather Macgowan, Pressure ulcer risk assessment & prevention guideline, NHS Forth Valley, Tissue Vialbility Team, 01.05.2020
2. Whitlock J. SSKIN bundle: preventing pressure damage across the health-care community.
British Journal of Community Nursing. 2014; 18:suppl 9: s32-39.
3. McCoulough S. Adapting a SSKIN bundle for carers to aid identification of pressure damage and ulcer risks in the community. British Journal of Community Nursing. 2016 June; Suppl:S19 – S25.
4. National Institute for Health and Care Excellence (2014) Pressure ulcers: prevention and management of pressure ulcers. NICE clinical guideline 179. NICE, London Overview | Pressure ulcers: prevention and management | Guidance | NICE
5. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The international Guideline. Emily Haesler (Ed.). EPUAP/NPIAP/PPPIA: 2019
6. Portoghese C et al. 2024. The Role of Shear Stress and Shear Strain in Pressure Injury Development.
7. Fletcher J. Pressure ulcer education 3: skin assessment and care, Nursing Times, December 2019, 115:12, 26-29
8. Pramod S. Mayes J. Bowling K. McDermott G., Implementation of skin tone assessment in pressure ulcer prevention, Wounds International 2024:15,1
9. Pressure Ulcers: Prevention and Management” Authors: National Pressure Injury Advisory Panel (NPIAP) Publication Year: 2019 Source: NPIAP Clinical Practice Guideline. Guidelines – National Pressure Ulcer Advisory Panel (npiap.com)
10. Parry Selina. M and Puthucheary Zudin A., The impact of extended bed rest on the musculoskeletal system in the critical care environment, Extreme Physiology & Medicine, 2015
11. Coleman S., Nixon J., Keen J., Wilson L., McGinnis E., Dealey C., Stubbs N., Farrin A., Dowding D., Scols J.M.G.A., Cuddigan J., Berlowitz D., Jude E., Vowden P., Schoonhoven L., Bader D.L., Gefen A., Oomens C.W.J. & Nelson E.A. (2014) A new pressure ulcer conceptual framework. Journal of Advanced Nursing, 2014
12. Jaul E., Barron J., Rosenzweig J. P., Menczel J., An overview of co-morbidities and the development of pressure ulcers among older adults, BMC Geriatr. 2018