How do pressure injuries occur?
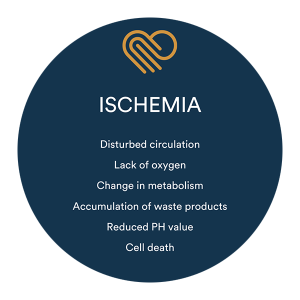
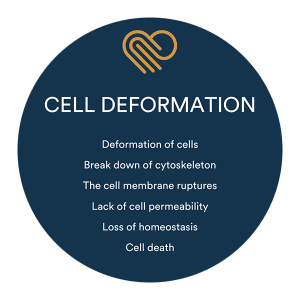
Ischemia has previously been widely recognized as the cause of pressure injuries and has historically been explained as the sole reason for their development. However, recent research has shown that there is another primary cause of pressure ulcers – cell deformation. Cell deformation typically involves higher and more intense pressure, while ischemia involves lower pressure that lasts for a longer period of time (1).